COVID-19 & Influenza: What You Need to Know
This article is part of an ongoing collaboration between the Colorado School of Public Health, the Denver Museum of Nature & Science, and the Institute for Science & Policy. Watch the full episode and find all of our previous COVID-19 webinars and recaps here.
COVID-19 and influenza are both highly contagious respiratory illnesses that can manifest with similar symptoms. With flu season returning to the U.S., scientists and public health officials are closely monitoring the overlap and bracing for additional strain on healthcare resources. As the two diseases set out on a possible collision course, how should we be assessing risk and adapting responsibly? And what measures can Coloradans take to mitigate the threat of a double whammy?
Recently, the Institute's Senior Policy Advisor Kristan Uhlenbrock compared and contrasted the flu and COVID-19 with Jon Andrus, MD, Adjunct Professor and Director of Division of Vaccines and Immunization at the Colorado School of Public Health, and Suchitra Rao, MD, Associate Professor of Infectious Diseases and Pediatrics at the Colorado School of Medicine.
This transcript has been edited and condensed for length and clarity. Watch the full recording here.
JON ANDRUS: I’m delighted and honored to be here, and just want to say up front what a pleasure it has been to work the last few years at the Center for Global Health, under the leadership of Dr. Steven Berman, who is the founding director and has really elevated the work there to a global level, making a difference.
So, I've been asked to provide some perspective on pandemics, and specifically on the COVID-19 pandemic. And I'd like to state up front that many of my reflections are based on my own experience. About 35 years ago, my first overseas assignment was to this hospital in Malawi, where I was asked to be the district medical officer as a Peace Corps volunteer. And although you see sinks in the operating room of the hospital built in 1908, there's no running water. The windows are broken. Flies and mosquitoes come in and out. There's no electricity. We were operating in filthy conditions out of the Wild West and I got a firsthand look at what can work in conditions like this. I don't think this is unusual in many of the developing countries around the world, at least in those that I've worked in.
I had the opportunity to oversee infectious diseases, particularly measles. We had a measles ward that often would have two or three patients per bed, and sometimes patients under the bed. Measles is a killer disease, and it's the most infectious virus on the planet. Fortunately, we have a vaccine, one of the better vaccines that we have to offer. So, out of this presentation and the discussion to follow, I hope I can leave you with the take-home message that vaccines in general are the most cost-effective interventions that medical science has to offer.
Having said that, not all vaccines are equal. Some vaccines are better than others. This particular vaccine for the most infectious virus on the planet happens to be a very good vaccine. And if we use it strategically based on the evidence, we can actually eliminate measles and it's one of the best buys in public health.
Now, polio is another infectious disease caused by a virus, but is not nearly as infectious as measles. In 1952, my former wife actually contracted polio. And it was terrifying to have these conditions where many children had to be put on iron lungs with 24/7 nursing to keep them alive. But we had a vaccine and, here again, using the strategies and tactics that we know work can actually also eradicate this disease,
Looking back at pandemics over the past century, 1918 is recognized as the mother of all pandemics. It caused the most devastation. (And I would not be here if my grandfather had not survived the 1918 pandemic while fighting in the trenches in France.) As you have heard, this outbreak was devastating, causing 50 to 100 million deaths worldwide. In the United States alone, there were 675,000 deaths, which was, by the way, 10 times the death rate of the war itself.
I want to highlight what happened in Philadelphia. To some extent, the virus subsided during the summer months, but on the 28th of September that year, there was a parade to raise funds to fight the war, and despite people stating the risk of such a parade, some hundred thousand people flocked to the streets of Philadelphia. Two days later, people were dropping like flies, and they ran out of coffins.
Fast forward to post-World War II and we have new challenges: nuclear proliferation, bioterrorism, and natural disasters related to climate change. An earthquake struck Haiti in 2010, killing thousands and thousands of Haitians and led to a subsequent cholera outbreak.
We've had some close calls. You've all heard about SARS and MERS. There's actually there is a silver lining to those outbreaks because of their contribution to the advancement of science that we're benefiting from vaccine development with the current pandemic. People don't often know or recognize that in 2004, there was an influenza virus that emerged in South Asia, the H5N1 virus. It only caused 400 cases, but had a case fatality rate of 60%. Think of that: six out of 10 people infected died. If that had gone global, that would have been disastrous. And the point here is that authorities use the information and attack the threat at its source. This virus emerged from poultry. So they went out and they slaughtered hundreds of millions of chickens in order to stop spread of the virus that had jumped to the human host, and with this case fatality rate.
We really need to maintain strong surveillance, not just in humans, but in animals as well where these viruses often emerge. It’s not always new pathogens. Pathogens that have been around, like dengue, a disease otherwise known as “break bone fever,” have increased rapidly since 1980 as a result of climate change and migration and urbanization. We've had outbreaks in Houston and Miami. These dengue cases disproportionately affect the poor whose homes that don't have air conditioning or screens to prevent mosquitos from entry into the home.
Vaccines are not all equal. They will have different safety profiles, some will work better than others. But how we use them will be very important. Strategies like aggressive masking and aggressive testing and contact tracing need to be promoted while the vaccine is being developed and even after the vaccine is introduced.
There are basically two pathways for vaccine development. The whole pathogen approach is a more traditional approach. We can take the pathogen and kill it, perhaps with formaldehyde or heat. In the case of inactivated polio vaccine, it’s a very effective vaccine. Or, we can attenuate the vaccine through cultures and other treatments that will soften the virus to still be live and still elicit an immune response as in the case of measles. The other pathway is the sub-unit pathway, which is actually critical to take advantage of and acknowledge the influence of the spike protein on the surface of the COVID virus. That will likely have a greater chance of being useful and may have fewer side effects. An example of this is the pneumococcal vaccine. You can take that protein and attach it to another to make it stronger, make it more effective, particularly in younger children. This is what I often refer to as a cut and paste technology.
There are many challenges to what I just listed. Documentation of the evidence is absolutely fundamental. In the United States, we have the FDA and the CDC and others working together to document safety and efficacy but then communicating so that we maintain public trust in the integration of the tool. The vaccine has to be used with the other public health interventions: masking, contact tracing, testing, avoiding crowds, all those things that you've been doing and following. It's not a magic bullet. And it won't be available all in one day.
SUCHITRA RAO: Thank you to Dr. Andrus, I really enjoyed hearing that historical context of pandemics. I am an infectious diseases physician, and I’m going to talk a little bit about what we can expect for our upcoming season, when we are faced for the first time ever with having a COVID-19 pandemic and influenza epidemic.
So, a little bit about some of the similarities and important distinctions. One of the most important factors is really going to be the extent of the crucial distance measures that are going to be in place. And I think that we can also see that the healthcare system has already been very overwhelmed. We have a situation where there could be both SARS-CoV-2 and influenza that are occurring at the same time. People can get infected with both at the same time. And a lot has to be learned about what that could look like and what that impact is.
Social distancing measures are probably going to be one of the most important factors. The other is the rate of influenza vaccination, or how well the population is covered against flu and how well that flu vaccine is working for that season. But then also that time period of when both will be circulating. We're going to see a peak of both viruses appearing at the same time.
We can make predictions about when we think the flu season will start, though the only thing that is predictable about the influenza season is its unpredictability. Looking at the last several seasons, they are really all over the map. Some of them have a very high peak, some of them have multiple peaks. Some of them go away quickly. And so there's really just a lot of variability within a given season in terms of calculating your flu season.
If we just focus on the last five seasons, we know that on average, the flu season lasts for about 16 weeks. And here in the United States, we usually see our peak around December to February. But we have seasons that start as early as November and could go out further — that really remains to be seen.
At the end of last season, with COVID 19 coexisting with influenza, you see this really sharp decline in the number of positive cases for flu. That's probably a result of social distancing mitigations put in place. We can also look to the Southern Hemisphere for clues. I’m originally from Melbourne, Australia, and I've been following their season very closely. There has been a complete flatlining of flu cases, and the mitigation strategies that they've been using over there have been a lot more than what we have. Melbourne, for example, just came out of a 16-week lockdown. This pattern has also been observed elsewhere in Chile, and in Africa. What it’s telling us, essentially, is that if we do have a further retightening of our social distancing measures, then this has the potential to flatten both the SARS-CoV-2 curve as well as the influenza curve.
It's really important to think about some of the similarities and then the important distinctions between influenza and COVID-19. Unfortunately, there's really no good way of distinguishing the two when you see people presenting with various signs and symptoms. Someone who has the flu can look very similar to COVID-19 and vice versa: cough, shortness of breath, muscle aches, nasal congestion and headaches. We've been hearing a lot about COVID-19 presenting with loss of taste or loss of smell, but it is important to remember that loss of smell has also been reported for viruses like influenza. And when you have a respiratory illness, it can impact your sense of taste but may not be a great distinguishing feature. I think with COVID-19, we have been seeing presentations with people having abdominal pain with diarrhea and vomiting, and that is something that has been described in influenza as well.
It’s important to also consider some of the complications that you can get from both COVID-19 and from flu. With influenza, you're much more likely to develop a secondary bacterial infection, things like pneumonia, sinus disease, ear infections in children, bloodstream infections. We know that people over the age of 65 are at the highest risk of having COVID-19. That is also true of flu, but remember that it is something that can really cause devastating disease in those who are under the age of five, and with the risk factors for infection, there's been a lot of similarities and overlap in the different medical conditions.
COVID carries extra risk when you have conditions like high blood pressure, obesity, diabetes and heart conditions. And then for influenza we do see it can also really have a heavy duty impact on those with weakened immune systems, and also with neurologic complications. It's been interesting to see some stark differences there. It seems more people having clotting complications with COVID-19. The issue of multi systemic inflammatory syndrome is more important for the COVID-19. One of the common complications has been muscle inflammation myositis.
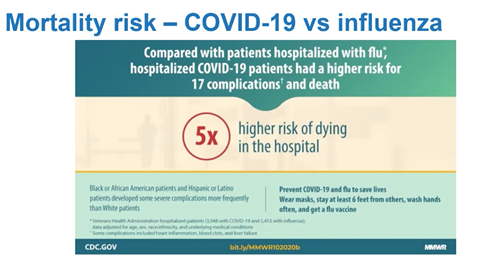 And then what about mortality rates? A paper that came out recently showed that there was a five times higher risk of dying in the hospital with COVID-19 than from influenza. But I really don't want folks to underestimate the impact of flu as well, especially as we're seeing both of these things appearing together for the upcoming season. Last season, it was estimated that influenza caused anywhere from 39 to 56 million flu illnesses and resulted in 18 million to 26 million flu visits to a provider that caused 110 to 740,000 hospitalizations, and it was estimated to have resulted in 24,000 to 62,000 deaths. So really staggering when you think about those things.
And then what about mortality rates? A paper that came out recently showed that there was a five times higher risk of dying in the hospital with COVID-19 than from influenza. But I really don't want folks to underestimate the impact of flu as well, especially as we're seeing both of these things appearing together for the upcoming season. Last season, it was estimated that influenza caused anywhere from 39 to 56 million flu illnesses and resulted in 18 million to 26 million flu visits to a provider that caused 110 to 740,000 hospitalizations, and it was estimated to have resulted in 24,000 to 62,000 deaths. So really staggering when you think about those things.
The other thing I'd like us to think about with influenza vaccines is how well they work. On average, vaccine effectiveness ranges from 40 to 60%. Flu vaccines are not necessarily going to be able to prevent you from getting the flu, like the measles vaccine can, but what it can do is prevent you from getting very sick. And so when you hear 40 to 60%, that's really telling you how well the flu vaccine prevents you from turning up to a doctor's office with symptoms of the flu.
Last season, influenza vaccination prevented seven and a half million illnesses, which is more than the population of Kentucky. It was able to prevent 105,000 hospitalizations, and that's enough people to fill the stadium at the University of Michigan. It also prevented 6,300 flu deaths, which is the equivalent to saving about 17 folks per day over the course of the year. Influenza vaccines can decrease your risk of being hospitalized by about 60%. It can decrease the risk of being admitted to the ICU by 80%. And it can decrease the risk of dying from the flu by 65%. The key factor for this season will be how much social distancing remains in place.
KRISTAN UHLENBROCK: Thank you, Suchitra. And to clarify: can a person have both influenza and COVID-19 at the same time?
SR: Yes, you can absolutely have both at the same time. A study out of China looked at a number of folks that were unfortunate enough to have both flu and COVID together, and it suggested that it may lead to worse disease. So those folks ended up being sicker, were in the hospital longer, and had worse outcomes. Right now, it's still a rare event. I think we'll learn a lot more about it in this upcoming season. But it is a little concerning that you can have both together.
KU: Would either of you like to comment on today’s Pfizer vaccine announcement, which is potentially 90% effective?
JA: My first reaction is that this is exciting. That particular study by Pfizer has some 40,000 study participants, which is a fair number. It's too early to say that there might not be a rare adverse event that you would see later, even after starting vaccination on a mass scale. You would need to monitor the safety profile and communicate it to the public to maintain trust. But I find it exciting.
I happen to sit on the advisory board of the Ministry of Health of Mexico where they're looking at the various vaccines that may be available for them. Messenger RNA is one, and they've been reviewing what would it take to have a successful distribution of this vaccine. Well, you need storage, you need a cold chain that is able to maintain it at 80 degrees Celsius below zero. And so you would need dry ice and other measures. They've found it quite challenging. It's not to say they can't do it, perhaps targeting cities, perhaps targeting the health care workers first. But the bottom line is, it's very exciting. We still need to keep our vigilance and monitor the safety concerns.
SR: I would just mirror that, in terms of this being very exciting. And, you know, early information. We know that the FDA, when they were coming up with their requirements of what would be considered an effective vaccine, they said 50%. So to see data that really well exceeds that to 90% is certainly very interesting, exciting information.
And it's important to keep in mind that there will be these early data that come out, where you sort of have these interim analyses. Show me what the effectiveness is at preventing infection. And I think that over time, these Phase III trials are really designed to look at some of the safety things that we will need to know over time after a vaccine is administered to these trial subjects. We need to continue to evaluate it even months and years later.
KU: Could you speak to the effectiveness of booster shots, particularly for those who are older?
SR: Yeah, that's a great question and I'm so glad this came up. What some data has been suggesting is the issue of waning immunity. So we know that immunity is very tricky, that the virus can mutate, that your antibodies that you develop may not last for the entire year. And they can go down over time. And we do notice that this is something that can happen if you are 65 years and older. If you get a flu vaccine in July or August, that may be too early. If you get a vaccine in September, we know on average it lasts for about six months and that should protect you for the flu season.
KU: Jon, could you talk a little bit about how important the collaboration with the World Health Organization is?
JA: My short answer is: absolutely critical. U.S. entities such as the CDC are globally recognized as being models of public health institutions, and to not have those dedicated workers at the table with other global experts is kind of like fighting the battle with two hands behind your back. You're not attending the meetings, you're not privy to some of the early discussion of results. So it's fundamental. Again, these viruses don't respect borders, so being able to collaborate among countries is also critically important. The global interrelations and relatedness of these diseases is obvious. For us not to be at the table is very sad.
As the former deputy director of the Pan American Health Organization, one of my jobs was to go up to Capitol Hill and brief people and their staff about the work that PAHO does. Before measles was eliminated in the Americas, most all the cases were imported from Latin America and the Caribbean, and now that is been taken care of. So it benefits us. If you look at the economic arguments as well, it's a tremendous value-added organization that the U.S. is a fundamental member of.
KU: What can any public health provider do to dispel myths and misinformation and really communicate truth around the safety, the effectiveness, the need, and the reliability of vaccines?
SR: I think that this is really becoming a huge issue. Historically, vaccines were really a public health celebration. They worked, they're effective, and they save lives. The scientific community and the civil rights community really need to do everything that we can to also be vocal about the importance of vaccines and about how safe they are. And I think to be fully transparent is really important as well. You've seen a lot of communication around that with developing the COVID-19 vaccine. They really want this to be a very transparent process to really make sure that the public is aware that yes, we're looking at the effectiveness of the vaccine, but we're also making sure that this is going to be safe, and that this is something that we can do safely.
But I think, just to break down that question a little bit, I think there's a few different things that we can do. I think one is to make sure that the scientific and medical community will have that information that they need to make sure that we can still continue to make a case for vaccines and how they work and the safety. I think second is things that you're doing, Kristan, you and your group — really give opportunities for us to be present, because like I said, you can sometimes just be overwhelmed by the amount of mistruths that are coming out.
JA: There are multiple ways of looking at this and simplifying things. Generally, people trust in their primary care provider. Dr. Sean O'Leary at the University of Colorado is doing a lot of research on how to communicate to patients and he's emerged as a global leader on this. His approach is to be proactive with your message as the patient enters the room and say hey, great, you're here for your vaccines today, rather than a more open ended traditional approach. People generally follow norms and then listen to their provider.
In a former life, I worked on polio eradication in India and I'll never forget going to Nepal and seeing a particular billboard. I asked a colleague to translate it. It was a person on a motorcycle with a leper — a clear leper, with the disfiguration. The other person on the bike was a famous comedian, hugging the leper to show to the public that you don't have to fear that person. It doesn't have to be stigmatized. So you can take advantage of community leaders. It may not be me, Jon Andrus, giving the message and in fact that may be counterproductive. But if you get Muhammad Ali, when he was alive, or Willie Mays, or this famous comedian...people tend to follow the norm. They did a study in college students that found that those that took the meningitis vaccine were more likely to take it if they knew that other students were taking it. So those are some of the strategies, I think, that will help benefit us as we go forward.
![]()
Disclosure statement:
The Institute for Science & Policy is committed to publishing diverse perspectives in order to advance civil discourse and productive dialogue. Views expressed by contributors do not necessarily reflect those of the Institute, the Denver Museum of Nature & Science, or its affiliates.

