COVID-19: Mid-Summer Update
This article is part of an ongoing collaboration between the Colorado School of Public Health, the Denver Museum of Nature & Science, and the Institute for Science & Policy. Watch the full recording of this session and find all of our previous COVID-19 webinars and recaps here.
Amidst a nationwide resurgence of COVID-19, Colorado scientists, health officials, and policymakers continue to closely monitor the disease’s status within the state. Mountain towns have seen an influx of summer visitors, bringing some economic relief, but also a rise in caseloads and concern that visitors will increase rates of infection. Counties are continuing to navigate physical distancing guidelines for businesses while warily looking ahead to opening schools in the fall. Face mask usage - recently mandated statewide - remains a political flashpoint. Five months into the coronavirus epidemic, what have we learned and where does Colorado go from here?
Recently, the Institute’s Senior Policy Advisor Kristan Uhlenbrock chatted with Jonathan Samet, MD, MS, Professor of Epidemiology and Environmental and Occupational Health and Dean of the Colorado School of Public Health. They were joined by John M. Douglas, Jr., MD, Executive Director of the Tri-County Health Department, and Karen Koenemann, Public Health Director for Pitkin County, for a discussion on how different areas of Colorado face different challenges in their respective public health responses.
This transcript has been condensed and edited for clarity and flow.
KRISTAN UHLENBROCK: Good morning everyone. Dr. Samet, could you start by giving us an update on the latest Colorado modeling?
JONATHAN SAMET: Thanks Kristan, and I’m pleased to see that we have some folks who’ve joined us for all of the sessions thus far. One of the measures we've been tracking is time spent at home, which also gives a look at mobility across the Denver metro area and the rest of Colorado. One thing we've learned is that mobility is a pretty good measure of how much we were mixing back in April and May, but now it's not quite as good now because we're doing different things. We're spending more time outside of our homes. We're going to stores or restaurants. So, things have changed a bit since the locked down months of March and April.
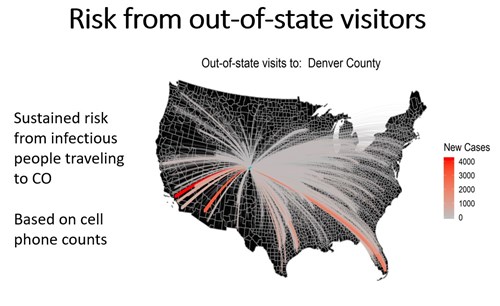 Now, this is certainly important for all our counties and particularly communities that have a lot of summer visitors like Pitkin County. This year, we bottomed out in April, as you would expect, and spent the most time at home. And now, visitors from out of state are rising. Part of the challenge for public health is that some of these folks are coming in from places that are hotspots like Florida, Texas, and California. Some of them may be coming in with infection. This epidemic is by no means static, and on-the-ground public health continually needs to adapt to what is going on.
Now, this is certainly important for all our counties and particularly communities that have a lot of summer visitors like Pitkin County. This year, we bottomed out in April, as you would expect, and spent the most time at home. And now, visitors from out of state are rising. Part of the challenge for public health is that some of these folks are coming in from places that are hotspots like Florida, Texas, and California. Some of them may be coming in with infection. This epidemic is by no means static, and on-the-ground public health continually needs to adapt to what is going on.
I think everybody knows that we're having rising numbers of cases in Colorado. Week over week, we had a 23% increase last week. Now, trends of cases are a little bit complicated because that number depends on how much testing we're doing. We are doing more testing, which will lead us to detect more cases, particularly among those who are asymptomatic. Another indicator is hospitalization, which our group tracks closely for the modeling. The big peak was back in mid-April, falling lower again in recent weeks, and now rising but with a plateau. Deaths are down and certainly nowhere near the peak, but we also know that there is a lag.
Colorado, like other states, is having a surge of cases in young people. The number of cases among 20 to 39 year olds is rising sharply and is now a majority of the cases we’re seeing. An important reminder here to those who are under 40: people in this age range do get symptomatic diseases and they can be sick enough to be in hospital and some have died.
As discussed last week, this epidemic has hit different groups within our population differently. We’ve seen high counts among those who are Black and African American, and also among those who are Hispanic or Latino. (The American Indian and Alaskan Native numbers bounce around a bit because it's a smaller population.) We see this disproportionate burden among people of color and that’s been such an unfortunate aspect of the pandemic across the country and across the world.
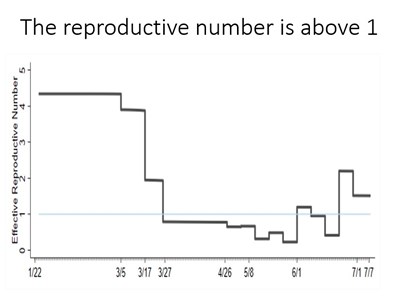 Our team has been doing infectious disease modeling in support of CDPHE and the Governor's office. We fit our models to the data and look both forward and backward to see how the epidemic propagates. One output of our models is the so-called reproductive number, or R0 (r-naught). The R0 value is the number of new cases per affected person. If that number is above one, an epidemic propagates. If it's below one, the epidemic is not going to propagate because each case does not make more than one additional case. So you can see the number, as we've calculated it over time, dropping below one in April and May as we were shut down. And then in recent weeks, it has been going back up and then maybe coming down again in the past week or two. This number is very important in terms of how well we’re doing in controlling the epidemic.
Our team has been doing infectious disease modeling in support of CDPHE and the Governor's office. We fit our models to the data and look both forward and backward to see how the epidemic propagates. One output of our models is the so-called reproductive number, or R0 (r-naught). The R0 value is the number of new cases per affected person. If that number is above one, an epidemic propagates. If it's below one, the epidemic is not going to propagate because each case does not make more than one additional case. So you can see the number, as we've calculated it over time, dropping below one in April and May as we were shut down. And then in recent weeks, it has been going back up and then maybe coming down again in the past week or two. This number is very important in terms of how well we’re doing in controlling the epidemic.
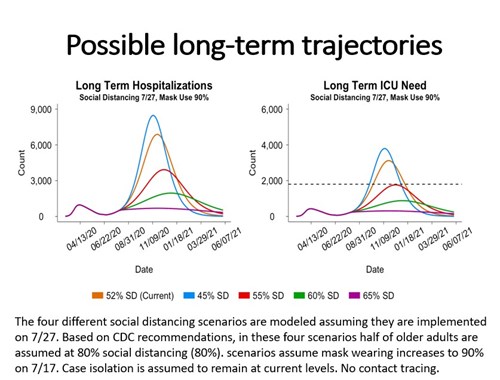 Here’s a projection for what we think might happen with hospitalizations and intensive care units. I've made some assumptions here around mask usage at 90%, continued public education about masks, and social distancing. We’re currently calculating that we’re at about 52% reduction in social interactions and as you can see on these plots, we don’t want to go over our ICU capacity to take care of patients (the dotted line in thee figure on the right). If we stay at 55% or better or get to 60% or 65%, we're doing well. I show you these upcoming months in detail because of course we're facing school openings and people returning to universities. The blue and orange trajectories are the ones that we want to avoid. Our models tell us that they could happen unless we maintain a sufficiently high degree of distancing.
Here’s a projection for what we think might happen with hospitalizations and intensive care units. I've made some assumptions here around mask usage at 90%, continued public education about masks, and social distancing. We’re currently calculating that we’re at about 52% reduction in social interactions and as you can see on these plots, we don’t want to go over our ICU capacity to take care of patients (the dotted line in thee figure on the right). If we stay at 55% or better or get to 60% or 65%, we're doing well. I show you these upcoming months in detail because of course we're facing school openings and people returning to universities. The blue and orange trajectories are the ones that we want to avoid. Our models tell us that they could happen unless we maintain a sufficiently high degree of distancing.
I want to reiterate again that masks work. There's a difference between epidemic curves with mask use at 70% and 90%. I would just urge those of you out there who have skepticism to know that they do make a difference. In the words of Governor Polis at his press conference a few weeks ago: “Wear a damn mask.”
KU: Thank you, Jon, and a follow-up right back to you: Could you talk a little bit more about modeling based on between different metrics, for example, hospitalizations?
JS: The answer is that there'll be different perspectives on this depending on what you're trying to accomplish. We've used the critical care threshold and hospitalization as a key metric because everyone wants to avoid running out of ICU beds. It’s a metric for giving policy guidance. We have tried to assure that we don't hit that critical threshold and to alert those at the state and local level. (We’ll hear in a moment what’s useful at a county level.) And of course, we want to avoid deaths. When they do happen, we do need to know who is dying in order to track demographics. So various measures have different roles in our decision making.
KU: Dr. Douglas, what’s happening over in Tri-County?
JOHN M. DOUGLAS, JR: Tri County – or Adams, Arapahoe, and Douglas Counties – makes up about a quarter of the state. So, not surprisingly, the trends that Dr. Samet mentioned are the ones we're seeing in our counties as well.
We had our low point in early June, and it's been up since then. We've seen some sawtooth-like trends, but I'd say generally that we continue to track cases because those are probably the most robust early indicator of what's happening with transmission. We do care about hospitalizations and deaths too and at least so far, we haven't seen those rise, which is obviously good news. I would say that's at least in part, if not in large part, due to the fact that it's the younger folks that are getting affected. I want to point out that not getting hospitalized or dying doesn't mean you do great. The CDC put out a report on Friday or Saturday that noted that about a third of the people who were outpatients were still feeling poorly after three weeks. And you might say, not a big deal. But a lot of those folks couldn't get back to work, they felt so poorly. So I think that hospitalizations and deaths are really critical, but they're not the full spectrum of illness.
The other thing I want to make a point about is schools. I believe we desperately want to see them open as much as possible. I think that not having schools open can have a huge impact on education. But again, if you have some not-so-sick individuals in the community transmitting infection, it won’t take many of those infections to close them right back down again.
KU: Karen, how are things going in Pitkin County?
KAREN KOENEMANN: Good morning, everyone. Pitkin County is located at the head of the Roaring Fork River Valley and Aspen is the county seat. Our workforce is really intertwined with Eagle County and Garfield County. So when we think about our case data, we really want to look at our whole region. As people are probably aware, tourism is a main driver of our economy, both in the winter and in the summer. Our census for Pitkin County has about 18,000 people, but right now we're estimating that we have about 39,000 to 42,000 people in our communities, so that really plays a role in how we think about our data and how we think about the strategies that we employ to try to manage disease transmission.
As of last night, we've had 153 cases and our positivity rate is ranging between 7 - 9% within the last week or so. We've had two deaths in Pitkin County since the start of the pandemic. We have a number of different indicators that we try to monitor, not just look at one. We look at disease burden, which includes a 14 day rolling case count, and our positivity rates. We look at our health care system capacities that includes inpatient hospitalizations, average daily visits, essential workers out of the hospital system with COVID-19, and then finally our disease control measures. We ask: what's our testing capacity, what's our timely case investigation, can we get through contact tracing and disease investigation within 24 hours, how many cases can we really track back to its original source?
We’re interested in using forefront data to to analyze what's happening and we've created a sort of thermometer-like alert system. Red is very high risk, orange is high risk. yellow is moderate, and blue is low. Right now, our community is in a yellow moving to orange. And then I’m looking at Eagle and Garfield and they’re actually both a little higher right now. We’re trying to track what's happening across the region and using that to inform our practices that we're implementing.
KU: I want to ask about testing, specifically the speed of getting results back quickly and how the delay can affect behavior.
JD: The testing issue is enormous. It's probably the single biggest problem we face in terms of trying to manage the epidemic right now. I believe in masks and I promote them, but getting good rapid turnaround testing is absolutely critical. Admiral [Brett] Giroir, who’s the head of the national testing task force, was on NPR this morning. He wants to get test results down to 24 hours or even less. I'll tell you that in the metro area right now, we're seeing tests that are averaging between five and 10 days. We're seeing some come back as late as 15 days. It's almost worthless, really, to have a test that comes back that late.
A recent study suggested that if you can't identify people for contact tracing within three days, the value just begins to plummet dramatically. If you're infected, you go into isolation to try to prevent other people from becoming exposed. If you're exposed but not infected, you go into quarantine or you try to stay away from other people. And when we can't identify people early for quarantine, it's really an enormous challenge. We really hope it gets better and the Governor is committed to taking steps to improve and we really appreciate his leadership in that area. I think as everybody's aware we're part of a global supply chain that you need to do tests: machines, pipettes, protective equipment, etc. And when India and Brazil and Texas and Florida are all competing for those items too, Colorado can see delays.
KK: We're seeing the same turnaround times here in Pitkin County. I think what's evolved and changed a little bit are the new kinds of PCR tests coming out and so we do have accessibility to a rapid format here. We see a faster time with our saliva testing, but for the normal swabbing testing, it's definitely slow as Dr. Douglas mentioned. When it’s slow, it’s not useful for us from a public health standpoint to continue with that disease investigation. We have created a regional testing strategy for Eagle, Garfield, and Pitkin and really prioritizing symptomatic people that have had direct contact and pose a high risk. That’s our framework right now and we don't have a lot of capability to really push other kinds of testing strategies for asymptomatic folks, just because we know that that test turnaround time is slow and we have to really prioritize others to get them into our disease investigation process.
KU: Karen, Pitkin’s population is often very fluid in the summer with tourists. What are some of your data showing on how tourists play into your caseloads, particularly those who are coming from hotspots?
KK: It’s actually a little bit complicated. We are primarily tracking our resident population, so we're looking at folks that have tested positive for COVID-19, get put into the state database and then we initiate a case investigation for those folks. If someone is from outside of the county or outside of the state, the investigation will be pushed to their place of residence.
We are able to track a little bit on those testing positive for COVID-19 illness who are not our residents. However, we don't do the full case investigation and follow up with those folks, so on a data front, we're still working really through the levels of detail for this. But what we do know right now is that we've been looking at the theoretical risk exposure to COVID-19 from commuters, tourists, and visitors depending on their origin. Through June 25, the risk exposure was 23% from Pitkin county residents and Garfield county residents was 20%. Folks from Texas, about 10%. We just did this analysis again last week. As of July 23, Texas was 21%, the rest of the US was 14%, and now Pitkin was 14%, so it just shows the impact of visitors. We adjust our strategies and our messaging for visitors so they're aware of what we're doing in our community to prevent disease transmission.
KU: Could you talk a little bit more about mobility data and understanding where people are coming from?
JS: We use mobility data to understand the impact of various measures, understand where people are mixing and the influx of visitors to the state. As bars and restaurants reopen, we looked at who was there and wee were able to get some insights. For example, the data showed that there were individuals in bars going on up until two in the morning, which is a time when food is likely not being served and perhaps people are not as physically distanced as they should be. So I think these data provide tracking monitoring and can highlight points where interventions may fail.
JD: Dean Samet is being modest in that his team has also done some fantastic work looking at mobility across counties. We don't just sit in our own county. We live and work and play and move to lots of different places. It’s not just Texas coming here, but people in Adams County who work in Denver or vice versa. And that's been extraordinarily important we think about policies to do a mask mandate. We've had a lot of experience in Tri-County in the last couple of weeks. To have a mandate in just a single county when people move around is just incredibly short sighted. That's why I think that, although the Governor likes to have matrix of both local and statewide policies, we’re one economy in some ways. We're clearly one healthcare system. If you get sick in Pitkin and that hospital starts to get overwhelmed you’re likely going to an ICU in the metro area. When we shop and work and travel, we're doing so in a way that doesn't respect jurisdictional boundaries.
KU: What has been valuable to you as far as coordination with other counties within the state?
JD: I think one of the successes that that I've experienced as a local public health director has in fact been regional collaboration with other public health entities. We have something in the metro area - a little bit like what Karen described for her neighbors in western Colorado – and we call ourselves the Metro Denver partnership. It's the counties in the metro area that we've been working quite closely together with terms of analytics. Dr. Samet comes and visits us frequently with his modeling updates.
We're really concerned about the testing situation. Lots of schools have, I think, have really good plans for testing. But I'm worried, especially with the big universities that may overwhelm the testing system even more. That’s where collaboration has been really useful. We've tried to message collaboratively. I think one of the things we've seen in this pandemic is just how much consistent messaging or, sadly, the lack of consistent messaging matters. And although I would have liked to have seen more consistent messaging nationally, I still think there's time to get there. I think we've been able to stay fairly on message in Colorado, in large part because of the sort of collaborative efforts that we've been able to undertake.
KK: We were one of the first counties to put in a public health order in March and it was one page. It limited group size to 50 people. Now, our public health order is 30 pages. We have mimicked the state public health order at times and we've had probably more restrictions than the state public health order. I'm really just trying to take a localized approach, especially with our unique economy in Pitkin County. But with that, I do think that the more we can do at a federal or state level and sync together is the most successful strategy. So when Governor Polis put in the statewide mask order, that gave us all more power. Every community has different levels of resources to go into fighting. The more we are aligned across the state, the more local communities and local health directors will be able to fulfill our objectives in the long run.
KU: What is one thing that you hope to see happening over the next couple of months, and one challenge that you're looking at?
JS: To name just a few, the schools and universities opening and the cold weather bringing us back indoors, where we'll be less distanced. Will our data systems provide us the early warnings that we need? John and Karen spoke to the critical need for having timely test results coming back. New data systems will be coming in to help. We've got to stay on top of things and look at leading indicators, not lagging indicators.
JD: I think schools will present challenges. As I said earlier, I really want to see them get going as much as possible. I think schools is a metaphor for the kind of balance we want to achieve. Some folks in the community are saying that we in public health are just shutting everybody down and all we care about is COVID. Let me say unequivocally that's not what we care about. We care about health across society. And I would note that when COVID has not been effectively addressed ─ look at Texas, Florida, Arizona ─ the economy does not do very well. So what we're trying to achieve is a fine-tuned balance.
I used to do vaccine research, so I am particularly biased toward vaccines as being a potential solution. It's worth noting that the first Phase III vaccine trial of one of the top four or five agents is going to begin enrollment today, including at the Anschutz campus. Early data published in the New England Journal of Medicine about three weeks ago looks really very encouraging in terms of immunity. And so I'm hopeful about that. But I don't want to take it for granted. We've got a healthy anti-vax or vaccine-hesitant movement in this country and I suspect that will probably play out again. Careful messaging and public trust are going to be a key ingredient as we try to manage the pandemic.
KK: Public health really is the route to social and economic recovery. The more we can get right on the political front, the faster we will get to where we want to be. As public health professionals, we recognize that the determinants of health play a role in someone's health outcome and that includes everything from access to great education to access to healthy food to access to employment.
If someone dies due to COVID-19, they don't have opportunity to come back. If someone loses their job, we recognize that that is a significant hardship for people, but hopefully we have systems in place that allow them to get a new job or have some supports economically until that happens. It’s a hard and difficult situation for everyone. Public health officials need to have real understanding of the hardships people are going through. These are not easy decisions. When we think about schools, we want to make sure that our community transmission in Pitkin County is low enough that schools can operate in a way that provides the best learning for kiddos. We have a responsibility as a community to ensure that happens. And that really is our goal right now: to have a successful winter season.


Former dean of the Colorado School of Public Health and Professor of Epidemiology and Occupational and Environmental Health
Disclosure statement:
The Institute for Science & Policy is committed to publishing diverse perspectives in order to advance civil discourse and productive dialogue. Views expressed by contributors do not necessarily reflect those of the Institute, the Denver Museum of Nature & Science, or its affiliates.

