The Summer of COVID-19
This article is part of an ongoing collaboration between the Colorado School of Public Health, the Denver Museum of Nature & Science, and the Institute for Science & Policy. Click here to watch the full recording of this session and find all of our previous COVID-19 webinars and recaps here.
COVID-19 has turned life upside-down in many ways over the past few months, and with summer officially set to begin next week, many Coloradans are now wondering what a season typically filled with swimming pools, backyard barbeques, and other warm weather activities will look like. To preview the season ahead, the Institute for Science & Policy’s Senior Policy Advisor Kristan Uhlenbrock chatted with Rachel Herlihy, MD, MPH, State Epidemiologist for the Colorado Department of Public Health & Environment and Jonathan Samet, MD, MS, Professor of Epidemiology and Environmental and Occupational Health and Dean of the Colorado School of Public Health.
KRISTAN UHLENBROCK: Welcome to you both. Could you give us an overview of the state of the epidemic in Colorado right now and what we should expect this summer?
DR. JONATHAN SAMET: We all certainly love to enjoy Colorado's spectacular beauty in the summer, whether that’s picnicking, hiking, or going to camp. This year, there are some things we may not be doing, like going to Red Rocks or Water World or some of these places where we gather in large numbers. We're not quite ready to do all of that yet.
Things are going well in Colorado. The number of people in hospital is going down steadily, which is good news. And the famous R0 (r-naught) number you've probably heard about, which represents the number of new infections per case, is below one. If that number were to rise above one, even to 1.1 or 1.2, that means that each person infected causes more than one additional case and the epidemic will propagate. So we're holding the epidemic in check as of the end of May, which is how far we can track that number at the moment.
We are moving around more than even just a few weeks ago. As Jude Bayham from CSU showed recently, we are now spending less and less time at home. We’re beginning to return to work and getting our badly needed haircuts and returning to other personal care services as well as traveling to restaurants that are open for carryout and now sit-down service. Visits to parks are increasing again as we start to take advantage of the Colorado summer. This is important and sets the stage for the need to continue on the good course that Colorado has been on.
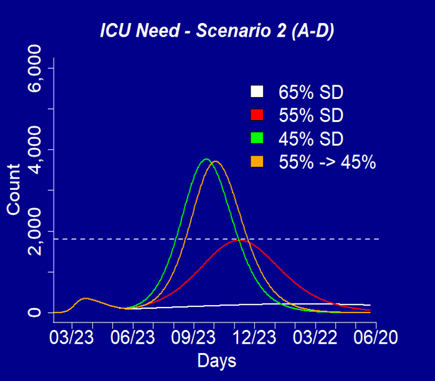 What can we project through the summer and into the fall? Here’s a look at the model we're using to predict the course of the epidemic in Colorado. The colors refer to different percentages of reduction of social distancing. For example, white would be a 65% reduction of contacts from where we used to be, or 45% in the green. And you can see our earlier peak. You hear a lot of talk about a second surge and if we don't maintain enough social distancing, these scenarios show that possibility.
What can we project through the summer and into the fall? Here’s a look at the model we're using to predict the course of the epidemic in Colorado. The colors refer to different percentages of reduction of social distancing. For example, white would be a 65% reduction of contacts from where we used to be, or 45% in the green. And you can see our earlier peak. You hear a lot of talk about a second surge and if we don't maintain enough social distancing, these scenarios show that possibility.
The dotted line going across is our ventilator capacity, basically our ability to take care of really sick people with COVID-19. These models assume current levels of mask wearing continue and case detection and isolation is increased 5% per week to 80% of symptomatic cases isolated.
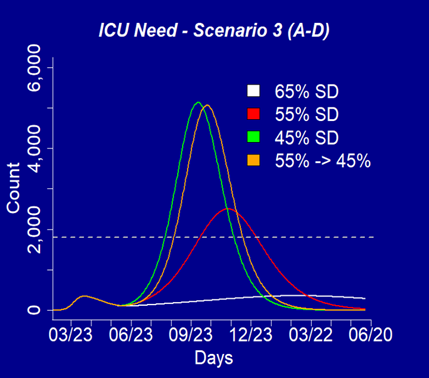 In Scenario 2, we've imagined that all people 65 and older maintain a high degree of social distancing. In Scenario 3, we've assumed that just about half of people 65 plus maintain a higher degree of social distancing. And you can see that to keep any possible second peak in check, we need to maximize that percentage.
In Scenario 2, we've imagined that all people 65 and older maintain a high degree of social distancing. In Scenario 3, we've assumed that just about half of people 65 plus maintain a higher degree of social distancing. And you can see that to keep any possible second peak in check, we need to maximize that percentage.
So what can we do as we head into the summer? Well, we can walk, hike, cycle, all those things. We can now go to restaurants able to open with up to 50% capacity inside and outside. We can swim in pools, we can go to gyms again ─ all with restrictions on the number of people ─ and some organized sports are allowed. Stores are open, although you'll see again lines outside as the numbers of people are limited. We are starting to open up, but we need to do it carefully.
DR. RACHEL HERLIHY: There are four key actions that I want to talk about here for Coloradans this summer. The first is practicing social distancing, particularly for older Coloradans. Second is wearing masks or cloth face coverings, third is getting tested, and fourth is supporting public health investigative work.
Risk of exposure to COVID-19 is really a numbers game. The more people you interact with, the more risk you have as an individual. One of the greatest challenges is asymptomatic transmission. We estimate that about 35% of infections are asymptomatic, which means people can be out and about and potentially transmitting this infection without any knowledge of being infected. A couple of weeks ago, the Governor started talking about an estimate of one in 300 Coloradans being actively infected with COVID-19. Thankfully, as we've seen a steady decline in the number of infections here in the state, we estimate that number is now probably closer to one in 600 or one in 700.
If you look at a facility like Red Rocks at full capacity, then we would estimate that between five and 10 asymptomatic individuals could potentially be there transmitting the virus to others. Similarly, if you look at the capacity of Coors Field, we could potentially have 25 to 50 people there who were asymptomatic. Mile High is even greater, with potentially 40 to 80 asymptomatic individuals. And that's why social distancing continues to be so important. To contain COVID-19, we really need people to have fewer interactions. So that might mean fewer backyard barbeques or perhaps those gatherings should be a little smaller than they were last summer.
It’s also critically important to continue to wear masks or cloth face coverings. We know that masks slow the spread of the virus by containing the wearer’s respiratory droplets. For someone who has an asymptomatic infection or a really mild infection, wearing a mask at the grocery store prevents that person from spreading the virus to someone else who may have a much more severe risk.
The other piece, of course, is to wear masks correctly. Wash your hands before and after putting a face covering or mask on and don’t touch your face again if possible. This is a challenge with children, especially young children. If your mask becomes soiled or hard to breathe through, it's time to remove it and launder it (the washing machine is just fine for cloth coverings). It's okay to remove your mask to eat and drink and if it's in good repair, you can continue to use it. The Colorado Mask Project allows you to purchase masks or you can make your own with instructions available on their website.
I want to talk a little bit about testing. At this point, we estimate that about half of symptomatic infections that are occurring in Colorado are being detected in the state. So if you think about being a boat that's leaking, we're trying to bail with a half-gallon bucket instead of a full gallon bucket. If we only know about half of the cases, we can really only act on that half. We think we can probably get to about 80% statewide. But if you have symptoms or meet criteria to get tested, make sure you're getting tested because that allows for more complete public health containment work.
Who should be tested? Any individuals who are symptomatic with fever, chills, cough, shortness of breath, difficulty breathing, fatigue, or muscle aches. One unique symptom of COVID-19 is a loss of taste or smell that comes on fairly suddenly. Other symptoms might be sore throat, congestion, runny nose, nausea, vomiting, or diarrhea. We also want individuals who are asymptomatic contacts to known cases to get tested about seven days after exposure so that those individuals may isolate and not transmit the infection to others. There's also a role for conducting ongoing testing for certain asymptomatic high risk workers, such as those who work in long term care facilities.
Supporting public health work can be a big help. There are multiple opportunities for the general public to get involved. The first is the Colorado symptom tracker, where you have the ability to report what you are experiencing and then receive information about what to do, including where to get tested. There's even an option to receive text messages and have public health officials check in with you to see how your symptoms are progressing over time.
You can also help us by “answering the call,” and this is related to a campaign that that CDC is working on to really help the public understand how case investigation and contact tracing work. If you're diagnosed with COVID-19, a public health worker will call you to ask about your symptoms and exposures to others. Your name will not be revealed to those that you came in contact with, even if they ask. And during that call, you'll be asked by public health to self-isolate for 10 days from onset of symptoms. We're asking the public to participate with us in this process.
Another example might be reaching out to contacts of a known case. If you are an individual who had contact with a confirmed case of COVID-19, which typically means being within six feet of a confirmed case for about 15 minutes, you might also get a call. A public health worker may call you to inform you of your exposure and you'll be instructed to stay home under quarantine for 14 days and monitor yourself for symptoms and seek testing if necessary.
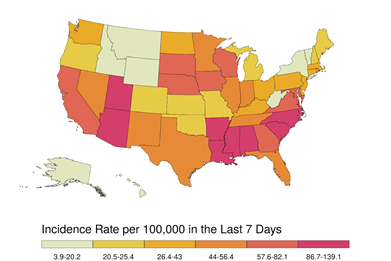 Finally, I want to just share a little bit of information about what's happening around the country and what's happening here in Colorado. So if you look at this map, you'll see that Colorado's case rate is quite low compared to some of our neighbors and this is really a reason to celebrate. We’ve done a great job of suppressing this virus by implementing social distancing, wearing masks, and taking all of the other measures that we know are important to prevent transmission. Unfortunately, quite a bit around us has changed in the last week. If you look at some of our surrounding states, their rates have increased quite substantially. So while we're feeling good here in Colorado, we know that we need to be cautious. We are seeing other states experience a resurgence of the virus and we want to do what we can to avoid that happening in Colorado.
Finally, I want to just share a little bit of information about what's happening around the country and what's happening here in Colorado. So if you look at this map, you'll see that Colorado's case rate is quite low compared to some of our neighbors and this is really a reason to celebrate. We’ve done a great job of suppressing this virus by implementing social distancing, wearing masks, and taking all of the other measures that we know are important to prevent transmission. Unfortunately, quite a bit around us has changed in the last week. If you look at some of our surrounding states, their rates have increased quite substantially. So while we're feeling good here in Colorado, we know that we need to be cautious. We are seeing other states experience a resurgence of the virus and we want to do what we can to avoid that happening in Colorado.
KU: Could you expand a little bit about what an increase in cases elsewhere means for Colorado, especially as people start traveling further this summer?
JS: Some of our earliest cases and hot spots were in the ski communities where we had high levels of mixing. For the past few months, we’ve been relatively isolated with little travel, so now it is a question of people coming in from out of state, some who may come from areas with higher rates of infection. Case identification and contact tracing are going to become much more important.
RH: We really need the help of the public to contain transmission of this virus and continue to practice high levels of social distancing. That number that Dr. Samet mentioned, with a target of a 65% reduction in social interactions, could be what this summer needs to look like. We certainly want people to be outside enjoying Colorado, being active, and seeing friends and family. But I think it's probably going to a bit less than normal with those precautions in place. If you're thinking about traveling I think the advice is: be cautious. Be respectful to the community you're going to. Be aware of what level of transmission is occurring in the place you're considering visiting. And then be cautious when you return as well and seek testing if you develop symptoms.
KU: The University of Washington’s Institute for Health Metrics & Evaluation recently said that Colorado was one of four states that could be one of the earliest for resurgence. Are you familiar with that model and why that might be the case?
JS: Our conclusions don’t always quite agree with theirs, but what happens now really depends on what we do. Our own model, which is really tailored to Colorado, presents a more favorable picture. But the biggest unknown is what our summer visitors may bring to us.
RH: I would echo that. I think there's a lot of unknowns and trying to predict when we're going to see an increase with absolute certainty is pretty difficult to do. There’s certainly risk here in Colorado and that's why we need to be diligent about maintaining our social distancing practices. We’re going to be paying close attention to the data so we have some early warning signs.
KU: Earlier, you mentioned that the R0 number is now below one. Does it matter how far below one it goes, and what kind of lag is there in the data?
JS: Keeping the R value below one is critical because you can from the projections that if it goes above that, those curves will begin to rise. We have a two week lag in understanding where we are. And that's because there are roughly two weeks from the time somebody becomes infected to when they may need hospitalization. Right now, in the middle of June, we're able to look back to what happened with measures taken through the end of May. We don't want to see that curve start to go up again because we know that if that happens, it's going to require a return to stricter measures. There are warnings coming from several states (New York, for example) where the epidemic came under control for a time and then social distancing decrease and that could lead to a second wave.
RH: As Dr. Samet mentioned, we’re always measuring about two weeks in the past. Today’s numbers that get posted on our website are really a reflection of exposures that occurred two weeks ago. It’s important to understand that when we’re acting on the data. We also aren't going to see the effect of changes and strategies until weeks later, which is another reason that we need to really be looking closely at the data and following it on a daily basis.
KU: How many symptoms should someone have before they go get tested?
RH: That’s one of the really challenging things about this virus: it presents differently in different individuals. I think that because some individuals are going to be asymptomatic, I would err on the side of caution if you have any suspicion of exposure. We’ve had individuals who only ever experienced a loss of tastes or smell, but were nevertheless carriers. We'd prefer that individuals are cautious at this period of time. It’ll be more challenging and more confusing as we move into the fall and we see other respiratory viruses circulating. It’ll be a challenging influenza season and it's particularly important this season for individuals to consider getting an influenza vaccine. There's going to be a lot of confusion about whether or not someone has influenza or COVID or something else. The more overall respiratory illnesses we can prevent, the better off our healthcare system in Colorado will be.
KU: Where can people go to get tested?
RH: It varies from community to community. A good first step is talking to your healthcare provider. You can also go to public health websites to get information on where testing locations.
KU: Does sunlight help keep COVID-19 at bay?
RH: We think that outdoor environments carry lower risk than being in indoor environments and there's probably a couple of reasons. The first is that it's generally easier to maintain social distancing. The second is that respiratory droplets are more likely to be rapidly dispersed and diluted, reducing risk of transmission to person from person.
JS: There is also some research underway on mask cleaning protocols using UV light, so perhaps there are other ways the power of sunlight can help, too.
KU: What is the current guidance on reopening places of worship, libraries, and other public venues that often accommodate larger groups and older populations?
RH: In general, as different types of businesses are opening, we need to ensure that social distancing is continuing as well as mask use. It’s particularly important for older Coloradans to be cautious and limit interactions with others where possible. For individuals that might be responsible for those businesses, I’d stress the importance of cleaning high touch surfaces.
JS: When we talk about droplet transmission, we're talking about bigger particles that don’t go too far outside of the six foot zone. There's nothing absolute about six feet, but it's a good approximation. So that means if people are in environments like, say, a house of worship, it's important that the distancing be maintained. That may make it hard to fill up some of places like they have been in the past. It’s similar to keeping the middle seat free on an airplane, which is not six feet and more like two feet, but it’s a start.
We still need more investigation into how we mix different age groups. On Sunday, for example, older people may spend a lot of time with younger people in houses of worship. As folks make decisions about where they're going to go, they should think about how much mixing might go on and whether it's really possible in different environments to adhere to this physical distancing for their own safety.
RH: There some places we have to go: work, childcare, the grocery store. But it’s worth thinking about those contacts with others that are not necessarily requirements. If you're thinking about how to modify your behavior and decrease your risk, it's probably starting with some of those things that that aren't absolute requirements. We obviously want people to be active and see family and friends. But some of those social interactions might be a place to modify your behavior a bit more than things that you're obligated to do on a daily or weekly basis.
KU: What effects could we see from ongoing demonstrations?
We know that when individuals are gathered in large numbers, there is potentially a risk of transmission. We want people to be able to express themselves, but it's just about making sure that it’s being done in a safe manner. Denver’s Mayor’s office has recommended that individuals who've been at protests get tested. The ideal time to do that is probably about a week after attendance, which is the time it takes for the virus to take hold. We are certainly paying close attention to the data. As I mentioned earlier, there is about a two week lag from the time of exposure until that data gets reported to public health officials. And at this point, we're not seeing increases that we could potentially attribute to protests that have occurred in Colorado, but yes, certainly anytime people gather, there is potential for increased risk of transmission.
KU: What about younger children, and specifically, playdates with other kids?
RH: One of the interesting thing about this virus is that children seem to have pretty mild infections. And kids are actually more likely to have asymptomatic infection (with some exceptions, such as newborns and those who have lung disease, asthma, or are otherwise immunosuppressed). In general, kids seem to be at lower risk than that older population and I think we're still learning more about their role in transmitting this virus to others.
In terms of playdates and interacting with others, I think it's probably the same rules that you use for your entire family: limiting the number of interactions. So perhaps one strategy would be to, you know, pick a couple of kids or small groups for your children to interact with and not necessarily a new friend every single day. That might limit the risk of transmission between households.
As far as school goes, I think there are still lots of unknown. I know that our school districts around the state are doing lots of work planning for a variety of scenarios. I think there's certainly a potential that we could see increased transmission in the fall. And so our schools are going to need to be prepared for that, and school could look different. We’re hopeful that we can get kids back in school. But in general, our new normal is going to be pretty different we have a vaccine or other treatment.
JS: Children have long been thought to introduce infections into in the households as they mix in school, thus infecting older people such as their parents and grandparents. We want to think about the strategies that will minimize risk as children begin to mix in groups in schools. Inevitably, some of them will bring infection home. The question will be how to protect the household and the broader extended networks as we head into the fall which could be a much more challenging time in so many respects that where we are now.
![]()

Former dean of the Colorado School of Public Health and Professor of Epidemiology and Occupational and Environmental Health

State Epidemiologist for the Colorado Department of Public Health & Environment
Disclosure statement:
The Institute for Science & Policy is committed to publishing diverse perspectives in order to advance civil discourse and productive dialogue. Views expressed by contributors do not necessarily reflect those of the Institute, the Denver Museum of Nature & Science, or its affiliates.
